BREAST CANCER IN MEN
Men with breast cancer may experience the following symptoms. Sometimes, men with breast cancer do not have any of these changes when diagnosed. Many times, the cause of breast changes may be another medical condition that is not cancer.
Talk with your doctor if you have the following signs or symptoms:
⦁ A lump that feels like a hard knot or a thickening in the breast or under the arm. Because men generally have small amounts of breast tissue, it is easier to feel a small lump.
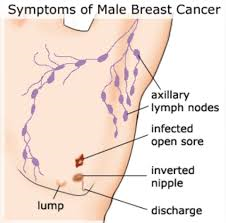
⦁ Any new irregularity on the skin or nipple, such as redness, scaliness, puckering, or a discharge from the nipple
If you are concerned about any changes you experience, please talk with your doctor. Your doctor will ask how long and how often you’ve been experiencing the symptom(s), in addition to other questions. This is to help find out the cause of the problem, called a diagnosis.
If cancer is diagnosed, relieving symptoms is an important part of cancer care and treatment. This may be called palliative care or supportive care. It is often started soon after diagnosis and continued throughout treatment. Be sure to talk with your health care team about symptoms you experience, including any new symptoms or a change in symptoms.
Doctors use many tests to find, or diagnose, cancer. They also do tests to learn if cancer has spread to another part of the body from where it started. If this happens, it is called metastasis. For example, imaging tests can show if the cancer has spread. Imaging tests show pictures of the inside of the body. Doctors may also do tests to learn which treatments could work best.
For most types of cancer, a biopsy is the only sure way for the doctor to know if an area of the body has cancer. In a biopsy, the doctor takes a small sample of tissue for testing in a laboratory. If a biopsy is not possible, the doctor may suggest other tests that will help make a diagnosis.
This section describes options for diagnosing this type of cancer. Not all tests listed below will be used for every person. Your doctor may consider these factors when choosing a diagnostic test:
⦁ The type of cancer suspected
⦁ Your signs and symptoms
⦁ Your age and general health
⦁ The results of earlier medical tests
In addition to a physical examination, the following tests may be used to diagnose breast cancer in men:
⦁ Clinical breast examination. During this procedure, the doctor will feel for lumps in the breast tissue and under the arm.
⦁ Diagnostic mammography. If a lump or suspicious area is found, the doctor will recommend a diagnostic mammogram
⦁ Ultrasound. An ultrasound uses high-frequency sound waves to create an image of the breast tissue. An ultrasound can distinguish between a solid mass, which may be cancer, and a fluid-filled cyst, which is usually not cancer.
⦁ Nipple discharge examination. Fluid from the nipple can be examined under a microscope to look for cancer cells.
⦁ Biopsy. A biopsy is the removal of a small amount of tissue for examination under a microscope. Other tests can suggest that cancer is present, but only a biopsy can make a definite diagnosis. A pathologist then analyzes the sample(s). A pathologist is a doctor who specializes in interpreting laboratory tests and evaluating cells, tissues, and organs to diagnose disease. There are different types of biopsies, classified by the technique and/or size of the needle used to collect the tissue sample.
⦁ A fine needle aspiration biopsy uses a thin needle to remove a small sample of cells.
⦁ A core needle biopsy uses a wider needle to remove a larger sample of tissue. This is usually the preferred type of biopsy to find out whether an abnormality on a physical examination or an imaging test is cancer. A vacuum-assisted biopsy removes several large cores of tissue. Local anesthesia, which is medication to block pain, is used to numb the area and lessen a patient’s discomfort during the procedure.

⦁ A surgical biopsy removes the largest amount of tissue. This biopsy may be incisional, which is the removal of part of the lump, or excisional, which is the removal of the entire lump. Because surgery is best done after a cancer is diagnosed, a surgical biopsy is usually not recommended to diagnose breast cancer. Most often, non-surgical core needle biopsies (see above) are used to diagnose breast cancer. This means that only 1 surgical procedure is usually needed after diagnosis to remove the tumor and to take samples of the lymph nodes.
⦁ Image-guided biopsy is used when a distinct lump cannot be felt, but an abnormality is seen with an imaging test, such as a mammogram. During this procedure, a needle is guided to the location with the help of an imaging scan, such as mammography, ultrasound, or Magnetic resonance imaging
⦁ A stereotactic biopsy is done using mammography to help guide the needle. A small metal clip may be put into the breast to mark where the biopsy sample was taken in case the tissue is cancerous and more surgery is needed. This clip is usually titanium so it will not cause problems with future imaging tests, but check with your doctor before you have additional imaging tests. An image-guided biopsy can be done using a fine needle, core, or vacuum-assisted biopsy (see above), depending on the amount of tissue being removed. Imaging tests may also be used to help do a biopsy on a lump that can be felt in order to help find the best location.
⦁ Sentinel lymph node biopsy is a way to find out if there is cancer in the lymph nodes near the breast. Learn more about sentinel lymph node biopsy in the The types of treatment section.
⦁ Analyzing the biopsy sample
Analyzing the sample(s) removed during the biopsy can help your doctor learn about specific features of a cancer that help determine treatment options.
⦁ Tumor features. Examination of the tumor under the microscope is used to determine if it is invasive or in situ, ductal or lobular, and whether the cancer has spread to the lymph nodes. The margins or edges of the tumor are also examined and their distance from the tumor is measured, which is called margin width.
⦁ ER and PR. Testing for ER and PR helps determine both the risk of recurrence and the type of treatment that is most likely to lower the risk of recurrence. ER and PR are often measured for DCIS as well. Generally, hormonal therapy is an option for ER-positive and/or PR-positive cancers.
⦁ HER2. The HER2 status helps determine whether drugs that target the HER2 receptor might help treat the cancer About half of HER2-positive tumors also have hormone receptors and can benefit from both hormone and HER2-targeted therapy.
⦁ Grade. The tumor grade is also determined from a biopsy. Grade describes how much cancer cells look like healthy cells when viewed under a microscope. The doctor compares the cancerous tissue with healthy tissue. Healthy tissue usually contains many different types of cells grouped together. If the cancer looks similar to healthy tissue and has different cell groupings, it is called "well differentiated" or a "low-grade tumor." If the cancerous tissue looks very different from healthy tissue, it is called "poorly differentiated" or a "high-grade tumor." The cancer’s grade may help the doctor predict how quickly the cancer will spread. In general, the lower the tumor’s grade, the better the chance that the cancer will not return.
⦁ Molecular testing of the tumor. Your doctor may recommend running other laboratory tests on a tumor sample to identify specific genes, proteins, and other factors unique to the tumor. If you have locally advanced or metastatic breast cancer, your doctor may recommend testing for the following molecular features:
⦁ PD-L1, which is found on the surface of cancer cells and some of the body's immune cells. This protein stops the body’s immune cells from destroying the cancer.
⦁ Microsatellite instability-high (MSI-H) or DNA mismatch repair deficiency (dMMR). Tumors that have MSI-H or dMMR have difficulty repairing damage to their DNA. This means that they develop many mutations or changes. These changes make abnormal proteins on the tumor cells that make it easier for immune cells to find and attack the tumor.
⦁ NTRK gene fusion, which is a specific genetic change found in a range of cancers, including breast cancer.
⦁ PI3KCA gene mutation, which is a specific genetic change commonly found in breast cancer.
Genomic tests to predict recurrence risk
Tests that take an even closer look at the biology of the tumor are commonly used to understand more about a breast cancer, particularly for a cancer that has not spread to other organs. These tests can help estimate the risk of cancer recurrence in the years after diagnosis. They can also predict whether a treatment will be helpful to reduce the risk of cancer recurrence. This helps some patients avoid the possible side effects of a treatment that is not likely to work well.
The tests described below are typically done on tissue removed during surgery. Most patients will not need an extra biopsy or more surgery. For more information about genomic tests, what they mean, and how the results might affect your treatment plan, talk with your doctor.
⦁ Oncotype Dx™. This test is an option for people with ER-positive and/or PR-positive, HER2-negative breast cancer that has not spread to the lymph nodes. This test can help patients and their doctors make decisions about whether chemotherapy should be added to hormonal therapy. This test looks at 16 cancer-related genes and 5 reference genes to calculate a “recurrence score” that estimates the risk of the cancer coming back within 10 years after diagnosis. The recurrence score is used to guide recommendations on the use of chemotherapy, which may also differ by age. It appears to provide equally helpful information for men as it does for women.
⦁ Mammaprint™. This test is an option for people with ER-positive and/or PR-positive, HER2-negative breast cancer that has not spread to the lymph nodes or has only spread to 1 to 3 lymph nodes. This test uses information from 70 genes to estimate the risk of recurrence for early-stage breast cancer. For people with a high risk of the cancer coming back, this test can help patients and their doctors make decisions about whether chemotherapy should be added to hormonal therapy. This test is not recommended for people with a low risk of the cancer coming back.
⦁ Additional tests. There are additional tests that may be options for people with ER-positive and/or PR-positive, HER2-negative breast cancer that has not spread to the lymph nodes. These tests include PAM50 (Prosigna™), EndoPredict, and uPA/PAI and can also be used to estimate how likely a cancer will spread to other parts of the body.
The tests listed above have not been shown to be useful to predict risk of recurrence for people with HER2-positive or triple-negative breast cancer. Therefore, none of these tests are currently recommended for breast cancer that is HER2 positive or triple negative. Your doctor will use other factors to help recommend treatment options for you.
Talk with your doctor for more information about genomic tests, what they mean, and how the results might affect your treatment plan.
Blood tests

The doctor may also need to do several types of blood tests to learn more about the cancer:
⦁ Complete blood count. A complete blood count or (CBC) is used to measure the number of different types of cells, such as red blood cells and white blood cells, in a sample of a person’s blood. It is done to check that your bone marrow is functioning well.
⦁ Serum chemistry. Serum chemistry tests are often done to look at minerals in your blood, such as potassium and sodium, and to evaluate kidney function. Serum chemistry may also include tests that evaluate the health of the liver.
Additional imaging tests
Additional imaging tests may not be done until after surgery. These tests are generally only recommended for patients with higher-stage disease. Most people with early-stage breast cancer do not need additional imaging tests.

Whether your doctor recommends imaging tests to find out if the cancer has spread depends on the following factors:
⦁ Your medical history and symptoms
⦁ The size and type of tumor in the breast
⦁ Whether the cancer has spread to lymph nodes
⦁ Results of your physical examination
The tests listed below may not be recommended for all patients. Talk with your doctor if you have questions about a specific test, including why it is or is not recommended.
⦁ X-ray. An x-ray is a way to create a picture of the structures inside of the body, using a small amount of radiation. A chest x-ray may be used to look for cancer that has spread from the breast to the lungs.
⦁ Bone scan. A bone scan may be used to look for spread of cancer to the bones. A radioactive dye or tracer is injected into a patient’s vein, and then the scan is performed several hours later using a special camera. The tracer collects in areas of the bone that are healing, which occurs in response to damage from the cancer cells. The areas where the tracer collects stand out on the image, compared to healthy bone, which appears lighter. Some cancers do not cause the same healing response and will not show up on the bone scan. Areas of advanced arthritis or healing after a fracture will also stand out.
⦁ Computed tomography (CT or CAT) scan. A CT Scan may be used to look for tumors in organs outside of the breast, such as the lung, liver, bone, and lymph nodes. A CT scan takes pictures of the inside of the body using x-rays taken from different angles. A computer combines these pictures into a detailed, 3-dimensional image that shows abnormalities, including most tumors. A CT scan can be used to measure the tumor’s size and find out if it is shrinking with treatment. A contrast dye may be injected into a patient’s vein before the scan to provide better detail.
⦁ Positron emission tomography (PET) scan. A Pet scan may also be used to find out whether the cancer has spread to organs outside of the breast. A PET scan is usually combined with a CT scan (see above). Similar to a CT scan, a PET scan is a way to create pictures of organs and tissues inside the body. A small amount of a radioactive sugar substance is injected into a patient’s vein. This sugar substance is then taken up by cells that use the most energy because they are actively dividing. Because cancer cells tend to use energy actively, they absorb more of the radioactive substance. A scanner then detects this substance to produce images of the inside of the body. Areas that are most active appear as bright spots, and the intensity of the brightness can be measured to better describe these areas. The CT scan combined with the PET scan may be used to measure the size of a tumor and to determine the location of the bright spots more accurately. A PET scan will also show any abnormalities in the bone, similar to the bone scan.
⦁ After diagnostic tests are completed, your doctor will review all of the results with you. If the diagnosis is cancer, these results also help the doctor describe the amount of cancer in the body. This is called staging. If there are suspicious areas found outside of the breast, you may need another biopsy, if possible, to confirm the diagnosis of cancer.

