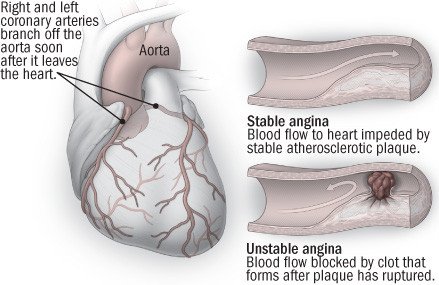
Angina is discomfort or pain in the chest that happens when not enough oxygen-rich blood reaches the muscle cells of the heart. The most common cause of angina is coronary artery disease. Coronary artery disease is usually caused by atherosclerosis. In this condition, fatty deposits (called plaque) build up along the inside walls of blood vessels that feed oxygen and nutrients to the pumping heart.
Angina occurs when one or more of the coronary arteries become narrowed or blocked. The discomfort of angina can be mild at first and gradually get worse. Or it may come on suddenly.
Although angina most commonly affects males who are middle-aged or older, it can occur in both sexes and in all age groups. Angina also is called angina pectoris.
Symptoms
Angina usually feels like a pressing, burning or squeezing pain in the chest. The main pain usually is under the breastbone. The pain may spread up toward the throat and into the jaw. The discomfort may be felt in the left arm and sometimes in both arms. People with angina often break out into a cold sweat. Other symptoms can include shortness of breath, lightheadedness and nausea.
Doctors divide angina into two types:
- Stable angina — Chest pain follows a specific pattern, occurring when someone engages in physical activity or experiences strong emotion. Exertion in cold weather or after a large meal is more likely to bring on angina. The symptoms should quickly subside once the person rests and relaxes.
Unstable angina — Symptoms are less predictable. This chest pain occurs at rest, during sleep or very often with minimal exertion. The discomfort may last and be intense. You should seek medical care immediately if this occurs, even if the chest pain has resolved.
Diagnosis
Your doctor may suspect that you have angina based on your symptoms and your risk of coronary artery disease. The doctor will review your medical history to see if you smoke (or have smoked) and whether you have diabetes and high blood pressure. Your doctor will ask about your family's medical history and will review your cholesterol levels, including LDL (bad) and HDL (good) cholesterol.
The doctor will check your blood pressure and pulse, and listen to your heart and lungs. You may need one or more diagnostic tests to determine if you have coronary artery disease. Possible tests include:
- Electrocardiogram (EKG) — An EKG is a record of your heart's electrical impulses. It can identify problems with heart rate and rhythm. Sometimes it can show changes indicating a blocked artery.
- Stress test — If your EKG is normal and you are able to walk, you'll be sent for an exercise stress test will be ordered. You'll walk on a treadmill while your heart rate is monitored. Other stress tests use medications to stimulate the heart, inject dyes to look for blockages and take ultrasound pictures to provide more information.
- Coronary angiogram — These X-rays of the coronary arteries are the most accurate way to measure the severity of coronary disease. A thin, long, flexible tube (called a catheter) is inserted into an artery in the forearm or groin. The doctor guides the catheter toward the heart using a special camera. Once the catheter is in position, dye is injected to show blood flow inside the coronary arteries, highlighting any areas that are narrow or blocked.
Expected Duration
An angina attack usually lasts less than five minutes. Pain that lasts longer than that or is severe may signal a more significant decrease in the heart's blood supply. This can happen when someone is having a heart attack or unstable angina.
Prevention
You can help to prevent angina caused by coronary artery disease by controlling your risk factors for clogged arteries:
- High cholesterol — Follow your doctor's guidelines for eating a diet low in fats and cholesterol and, if necessary, take medication to decrease your cholesterol.
- High blood pressure — Follow your doctor's recommendations for changing your diet and taking your medication.
- Smoking — If you smoke, quit. If you don't smoke, don't start.
- Diabetes — Test your blood sugar frequently, follow your special diet, and take your insulin or oral medication as your doctor has prescribed.
It's also wise to exercise regularly and to maintain an ideal weight. If angina attacks are triggered by emotional stress, learning stress management or relaxation techniques may be helpful.
Treatment
When angina is caused by coronary artery disease, treatment usually includes:
- Lifestyle changes — Changes include weight loss for obese patients, therapy to quit smoking, medications to lower high cholesterol, a program of regular exercise to lower high blood pressure, and stress reduction techniques.
- Nitrates, including nitroglycerin — Nitrates are medications that widen blood vessels (vasodilators). They increase blood flow in the coronary arteries, and make it easier for the heart to pump blood to the rest of the body.
- Statins, such as atorvastatin (Lipitor), rosuvastatin (Crestor) and simvastatin (Zocor, generic versions) - - These medications lower cholesterol, slow the rate of fatty buildup in the coronary arteries and decrease the risk of heart attack.
- Beta-blockers, such as atenolol (Tenormin) and metoprolol (Lopressor, Toprol-XL) — These medications decrease the heart's workload by slowing the heart rate and reducing the force of the heart's contractions, especially during exercise.
- Aspirin — Because aspirin helps to prevent blood clots from forming inside narrowed coronary arteries, it can reduce the risk of heart attacks in people who already have coronary artery disease.
If lifestyle changes and drugs fail to ease angina or when the risk of heart attack is great, your doctor may recommend balloon angioplasty or coronary artery bypass surgery.
When To Call a Professional
Call your doctor if you experience chest pains, even if you think you are too young to have angina and have no history of heart problems in your family. Your doctor will recommend the next steps based on how you describe your symptoms and risk factors.
Prognosis
In people with coronary artery disease, the outlook depends upon many factors, including the location and severity of the artery narrowing, and the number of coronary arteries involved. Proper treatment greatly improves the outlook for people with coronary artery disease.
