
In obsessive-compulsive disorder (OCD), a person is troubled by intrusive, distressing thoughts (obsessions) and feels the pressure to carry out repetitive behaviors (compulsions).
Neuroscientists believe that the brain pathways involved with judgment, planning and body movement are altered in OCD. Environmental influences, such as family relationships or stressful events, can trigger or worsen OCD symptoms.
OCD affects up to 3% of people worldwide. A childhood onset form can start around 10 years of age, more commonly in boys than girls. Most of the remainder of people with OCD have their first symptoms before they turn 25 — in this group, women outnumber men. OCD symptoms don't usually develop after age 30.
There is strong evidence that the illness has a genetic (inherited) basis, particularly in the childhood onset type.
Sometimes people with OCD manage their obsessions without giving any external sign that they are suffering. Usually, however, they try to relieve their obsessions by performing some type of compulsion: a repeated behavior or mental action that is aimed at soothing the fears. For example, a woman who has the obsession that her hands are dirty may develop the compulsion to wash them 50 times a day. A man who fears that his front door is unlocked may feel compelled to check the lock 10 or 20 times each night.
Symptoms
The two defining symptoms of OCD are obsessive thoughts and compulsive actions. The symptoms are bad enough to be time-consuming, cause functional impairment or be significantly distressing.
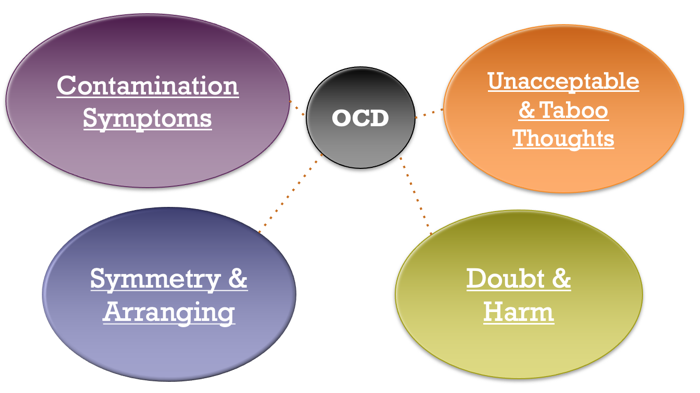
Obsessions are persistent, repeated, anxiety-provoking or distressing thoughts that intrude into a person's consciousness. Obsessions vary and can relate to any kind of fear. Here are some common ones:
- Fear of contamination – Constant worry about having dirty hands or clothing, or about catching or spreading germs.
- Fears related to accidents or acts of violence – Fear about becoming a victim of violence (an unlocked door that admits an intruder) or suffering accidental bodily harm (an oven is not turned off or a cigarette is not properly snuffed out).
- Fear of committing an act of violence or sexual misconduct – Fear of losing control and doing harm to others, or committing a harmful or embarrassing sexual act. For example, a loving mother worrying about suffocating her infant, or a respectable businessman fearing he will take off his clothes in a meeting.
- Fears that center on disorder or asymmetry – An irresistible need for order, anxiety about the smallest out of place detail. Examples are socks not being aligned "properly" in a drawer or food arranged "incorrectly" on a dinner plate.
Often, an adult with OCD will recognize that the obsessive thoughts are not realistic and will try to ignore them or suppress them. Temporary relief may come by performing a compulsive action.
Compulsions are persistent, repetitive behaviors or mental acts. The goal is to reduce the anxiety caused by obsessive thoughts. The compulsions are not realistically connected to the source of anxiety. Examples include:
- Repeated washing or bathing
- Refusal to shake hands or touch doorknobs
- Repeated checking of locks or stoves
- Compulsive counting of objects
- Over-organizing of work or household items
- Eating items of food in a specific order
- Repeating specific words or prayers
Anyone may feel compelled to recheck a locked door or wash hands to assure cleanliness. By themselves, such behaviors do not mean a person has OCD.
In OCD, the obsessions and compulsions are excessive and distressing. They are time-consuming, sometimes eating up several hours each day. They may interfere with personal relationships, as well as performance at work or school. Some compulsions may cause physical injury. For example, compulsive hand washing can lead to chapped hands and dermatitis, while excessive tooth brushing can cause torn, bleeding gums.
Diagnosis
Some people with OCD seek help from a primary care physician when symptoms begin to affect their health or interfere with life. An adult with compulsive hand washing may visit a dermatologist because of cracked, bleeding fingers, or a parent may consult a pediatrician when a child with OCD begins to be controlled by particularly intense rituals (for example, counting or checking).
Depressed mood is very common in OCD. In fact, a person may talk about feeling depressed instead of discussing OCD symptoms that are embarrassing or otherwise difficult to describe.
Your primary care doctor will likely refer you to a mental health professional for evaluation and treatment.
A mental health clinician will diagnose OCD by asking you about
- Obsessive thoughts and compulsive behaviors
- Psychological distress
- Consequences in important relationships
- Consequences at work and play
- Possible symptoms of other psychiatric illness

Most people with OCD know that their thoughts and behaviors are unrealistic. A significant minority have poor insight into their symptoms and a few have no insight. OCD with poor or no insight is harder to treat.
A significant minority of people with OCD have symptoms of a tic disorder or may have had a tic disorder in the past.
Expected Duration
OCD rarely disappears spontaneously, and the symptoms may last for years if not treated properly. In fact, it is common for a person with OCD to have the problem for 5 to 10 years before seeing a psychiatrist. Getting help sooner can reduce the impact of the illness.
Prevention
There is no way to prevent OCD, but the negative effects can be limited if the illness is detected and treated early.
Treatment
The most effective treatment for OCD is to combine psychotherapy and medications.
Your doctor may also offer treatment for any other conditions that may be contributing to the problem, such as a medical problem or depression. You may need to try more than one approach before you find the one that is right for you.
Psychotherapy
A number of psychotherapy techniques may be helpful, depending on the person's preference, events that may have triggered the problem, and the availability of family and other social support. It's important for a person suffering with OCD to be educated about the illness and to get support from friends, family or support groups.
The available research suggests that exposure and response prevention (ERP) and cognitive behavior therapy (CBT) work best. CBT is designed to help a person with OCD recognize the unreasonableness of the fearful, obsessive thinking. ERP is one of several techniques aimed at extinguishing compulsions.
- Exposure and response prevention (ERP) – A person is exposed to situations that provoke obsessive thoughts. He or she is then prevented from performing the usual compulsive action. For example, a person may be asked to touch a "dirty" shoe, and then be told to wait before washing his or her hands. The person will practice this behavior daily, gradually increasing the waiting time and keeping a diary of his or her efforts.
- Habit reversal – A person is asked to substitute a different response, such as deep breathing or fist clenching, for the usual compulsive action.
- Thought stopping – The person uses some form of distraction whenever an obsessive thought occurs. One common method is to say the word, "Stop," and snap a rubber band that's worn at the wrist.
- Saturation – The person concentrates intensely on the obsessive thought until the thought loses its impact and becomes meaningless.
Psychodynamic, insight-oriented or interpersonal psychotherapy can help a person sort out conflicts in important relationships or explore the history behind the symptoms, though insight itself is not likely to have an impact on severe symptoms.
Family therapy and group therapy also have been used in OCD. Since this disorder can be very disruptive to family life, family therapy may be particularly helpful.
Antidepressant Medications
Some antidepressants are effective for obsessive-compulsive disorder. Doses used are usually higher than the doses used to treat other illnesses like depression or anxiety. It also commonly takes longer before a person gets relief.
Selective serotonin reuptake inhibitors (SSRIs), such as fluvoxamine (Luvox), fluoxetine (Prozac), sertraline (Zoloft), paroxetine (Paxil), citalopram (Celexa) and escitalopram (Lexapro) are most commonly used.
Tricyclic antidepressants also can be effective. The one most used for OCD is clomipramine (Anafranil). Although this drug may be slightly more effective than the SSRIs for treating OCD, it sometimes has side effects that are more difficult to tolerate. Nonetheless, it is a good option.
Especially for people with poor or no insight into their illness, the doctor may offer an antipsychotic medication in addition to an antidepressant. Possible options are risperidone (Risperdal) and aripiprazole (Abilify). Such medications may also be used for severe OCD that hasn't gotten better with antidepressant treatment.
Medications: What to consider:
Here are some issues to discuss with your doctor about medications for OCD:
- Choosing a medication. In general, the goal is to effectively control symptoms at the lowest possible dosage. It's not unusual to try several drugs before finding one that works well. Your doctor might recommend more than one medication to effectively manage your symptoms. It can take weeks to months after starting a medication to notice an improvement in symptoms.
- Side effects. All psychiatric medications have potential side effects. Talk to your doctor about possible side effects and about any health monitoring needed while taking psychiatric drugs. And let your doctor know if you experience troubling side effects.
- Suicide risk. Most antidepressants are generally safe, but the FDA requires that all antidepressants carry black box warnings, the strictest warnings for prescriptions. In some cases, children, teenagers and young adults under 25 may have an increase in suicidal thoughts or behavior when taking antidepressants, especially in the first few weeks after starting or when the dose is changed. If suicidal thoughts occur, immediately contact your doctor or get emergency help. Keep in mind that antidepressants are more likely to reduce suicide risk in the long run by improving mood.
- Interactions with other substances. When taking an antidepressant, tell your doctor about any other prescription or over-the-counter medications, herbs or other supplements you take. Some antidepressants can make some other medications less effective and cause dangerous reactions when combined with certain medications or herbal supplements.
- Stopping antidepressants. Antidepressants aren't considered addictive, but sometimes physical dependence (which is different from addiction) can occur. So stopping treatment abruptly or missing several doses can cause withdrawal-like symptoms, sometimes called discontinuation syndrome. Don't stop taking your medication without talking to your doctor, even if you're feeling better — you may have a relapse of OCD symptoms. Work with your doctor to gradually and safely decrease your dose.
Neurostimulation
Deep-brain stimulation is used in the rare cases when OCD is resistant to all of the above treatments. In this technique, a neurosurgeon implants ultra-thin electrodes deep in the brain in order to stimulate a specific region thought to be involved with OCD symptoms.
This treatment is only offered for a person who has persistent incapacitating symptoms after receiving several ERP sessions, several adequate trials of antidepressants and augmentation with an antipsychotic.
When To Call a Professional
Since the symptoms of OCD seldom disappear without treatment, you should contact your primary care doctor whenever obsessive thoughts or compulsions cause you significant distress or discomfort, interfere with your ability to have a normal life at home or work, or cause you injury. Your primary care doctor will refer you to a psychiatrist for appropriate and effective treatment.
The most effective treatments for OCD are Cognitive Behavior Therapy (CBT) and/or medication. More specifically, the most effective treatments are a type of CBT called Exposure and Response Prevention (ERP), which has the strongest evidence supporting its use in the treatment of OCD, and/or a class of medications called serotonin reuptake inhibitors, or SRIs.
Exposure and Response Prevention is typically done by a licensed mental health professional (such as a psychologist, social worker, or mental health counselor) in an outpatient setting. This means you visit your therapist’s office at a set appointment time once or a few times a week.
Medications can only be prescribed by a licensed medical professionals (such as your physician or a psychiatrist), who would ideally work together with your therapist to develop a treatment plan.
Taken together, ERP and medication are considered the “first-line” treatments for OCD. In other words, START HERE! About 70% of people will benefit from ERP and/or medication for their OCD.
Diagnosis
Steps to help diagnose obsessive-compulsive disorder may include:
- Psychological evaluation. This includes discussing your thoughts, feelings, symptoms and behavior patterns to determine if you have obsessions or compulsive behaviors that interfere with your quality of life. With your permission, this may include talking to your family or friends.
- Diagnostic criteria for OCD. Your doctor may use criteria in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), published by the American Psychiatric Association.
- Physical exam. This may be done to help rule out other problems that could be causing your symptoms and to check for any related complications.
Diagnostic challenges
It's sometimes difficult to diagnose OCD because symptoms can be similar to those of obsessive-compulsive personality disorder, anxiety disorders, depression, schizophrenia or other mental health disorders. And it's possible to have both OCD and another mental health disorder. Work with your doctor so that you can get the appropriate diagnosis and treatment.
Prognosis
Since OCD can be a chronic (long-lasting) condition, ongoing treatment may be necessary.
The outlook however is good. Most patients improve and some recover completely.
