.jpg)
Vaginal cancer is the uncontrolled growth of abnormal cells in the vagina (birth canal) the muscular tube that connects your uterus with your outer genitals. Vaginal cancer most commonly occurs in the cells that line the surface of your vagina, which is sometimes called the birth canal.

While several types of cancer can spread to your vagina from other places in your body, cancer that begins in your vagina (primary vaginal cancer) is rare.
Cancer that starts in the vagina is called primary vaginal cancer. Primary vaginal cancer is rare. More commonly, cancer cells in the vagina are from cancer that started somewhere else, such as the cervix. There are two main types of primary vaginal cancer: squamous cell carcinoma and adenocarcinoma.
The vast majority of vaginal cancers are squamous cell carcinomas. These cancers arise from the surface of the lining of the vagina. They usually develop slowly, most often in the upper part of the vagina near the cervix. This type of cancer typically affects women between 50 and 70 years old.
Adenocarcinomas form in the glands in the vaginal wall. This type of cancer is much less common than squamous cell carcinoma. However, it is the most common type of vaginal cancer in women younger than 20 years old. Daughters of mothers who took the drug diethylstilbestrol (DES) while pregnant have a higher risk of developing this rare form of cancer. (DES, introduced in the 1940s to help prevent miscarriages, was banned in the United States in 1971.)
Doctors recently identified vaginal lesions that are not cancerous. These lesions are called vaginal intraepithelial neoplasia, or VAIN. Having VAIN may make a woman more likely to develop cancer. VAIN is associated with human papilloma virus (HPV) infections. HPV infection can also lead to cervical, anal, and throat cancers.
Less common types of vaginal cancer include malignant melanomas and sarcomas. Melanomas tend to affect the lower or outer part of the vagina. Sarcomas develop deep in the vaginal wall.

Symptoms
Symptoms of vaginal cancer include:
- abnormal vaginal bleeding, often after sex, that is not related to your period
- unusual vaginal discharge
- a mass that can be felt
- pain during sex
- pain in the pelvis
- painful urination and constipation.
These symptoms also occur in several less dangerous—and more common—conditions, such as infections of the reproductive organs. But these symptoms should always be evaluated by a doctor.
In some cases, a woman may not have any symptoms. Instead, the disease is found during a routine exam.

Diagnosis
Your doctor will ask about your medical history, symptoms, and risk factors for vaginal cancer. He or she will then perform an internal pelvic exam and Pap smear. During a Pap smear, a small plastic stick and soft brush are used to collect cells from the vagina and cervix. These cells are examined for abnormalities.

If the exam or Pap smear shows any abnormalities, your doctor will do a colposcopy. During this exam, he or she will look at the cervix and walls of the vagina with a magnifying lens. Small bits of tissue may be removed and checked for cancer cells in a laboratory. This is called a biopsy.
If cancer is diagnosed, your doctor may perform imaging tests to determine whether the cancer has spread and, if so, how far. These may include
- an x-ray of the colon (with a barium enema to help highlight the colon)
- computed tomography (CT) scans, to see cross-sectional images of organs and tissues
- magnetic resonance imaging, for detailed pictures of lymph nodes and other organs
- x-rays of the chest and other bones.
You may also have endoscopic tests. During these tests, your doctor can view the inside of the bladder, rectum, and part of the colon through a tube with a tiny camera on the end.

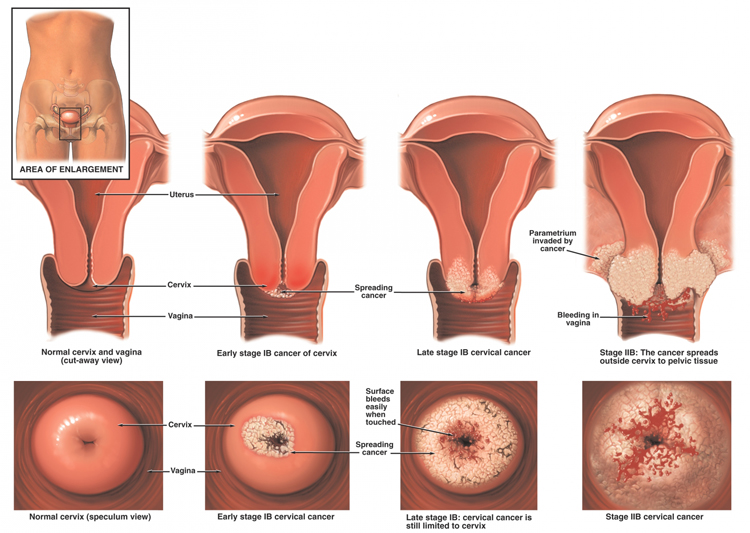
Doctors assign a numerical stage to cancer. The stage indicates how far the cancer has spread. These are the stages of vaginal cancer:
- Stage 0. This is a very early stage. Cancer is only on the surface of the vagina.
- Stage I. Cancer is confined to the vagina, but it penetrates beneath the surface.
- Stage II. Cancer has spread to the tissues just beyond the vagina, but not to the pelvic wall or other organs.
- Stage III. Cancer has spread to the pelvic bones and/or other organs and lymph nodes in the pelvis. The affected lymph nodes are on the same side of the body as the tumor.
- Stage IVA. Cancer has spread to the rectum and bladder. Lymph nodes on both sides of the body may be affected.
- Stage IVB. Cancer has spread to other parts of the body, such as the lungs.
- Recurrent. Cancer has come back after having been treated. It can affect the vagina or other parts of the body.
Expected Duration
Unless treated, vaginal cancer continues to grow and spread.
Prevention
To lower your risk of vaginal cancer, follow these guidelines:
Avoid human papilloma virus (HPV) infection. HPV is a common sexually transmitted disease that causes genital warts. Certain types of HPV are associated with cervical and vaginal cancer. If:
- the vagina or cervix gets infected with HPV, cells can grow abnormally. This increases the chance of developing squamous cell cancer.
The risk of HPV infection increases if you begin having sex at an early age. The risk also increases if you have unprotected sex, have many sex partners, or have sex with a person who has had many partners.
To avoid HPV infection, always use condoms and limit your number of partners. Condoms cannot always prevent HPV infection, but they can lower the risk of HIV and other sexually transmitted diseases. - Get regular Pap tests. Many vaginal squamous cell cancers develop from changes in the surface of the vagina. These changes can be detected by a Pap test and treated before full cancer develops.
In general, doctors recommend that a woman start to have annual Pap tests before she becomes sexually active or by age 21 at the latest. After three negative Pap tests, your doctor may do the test every two to three years. (This will depend on your age and your risk of developing cervical cancer.) Women older than 40 should continue to have an annual pelvic exam. - Do not smoke. Women with vaginal cancer have an increased risk of lung cancer. Since lung cancer is related primarily to tobacco use, smoking and vaginal cancer may be linked.
- Tell your doctor if your mother or grandmother took DES. He or she may want to monitor you more closely for VAIN and other conditions.
Treatment
The choice of treatment depends upon the type of cancer and its stage. The treatment plan also takes into account a woman's age, overall health, fertility, and personal preferences.
The two main treatments for vaginal cancer are radiation therapy and surgery. Chemotherapy has not proven to be very successful for vaginal cancer. It is only used for very advanced cancers (with or without radiation), and then usually as part of a clinical trial.
Various types of radiation therapy may be used. These include external-beam radiation, internal radiation, or a combination. External-beam radiation involves carefully targeting a beam of radiation at the cancer from a machine outside of the body. Internal radiation therapy, also called brachytherapy, involves placing radioactive materials inside the vagina. While external-beam radiation can harm nearby healthy tissues, brachytherapy can cause more vaginal side effects, such as scarring of vaginal tissues.
There are two other types of internal radiation therapy. Low-dose brachytherapy involves placing radioactive material inside a cylindrical container, which is placed in the vagina for one to two days. Interstitial therapy involves placing radioactive materials directly into the cancer with needles.
Only a small number of vaginal cancers are treated with surgery. That's because the surgery tends to be extensive. Plus, it may not be any more effective than radiation therapy. One exception: Stage I adenocarcinomas. In these cases, doctors may remove the tumor, some surrounding tissue, and the lymph nodes. This limited operation may be followed by radiation therapy. This type of treatment can help preserve a woman's fertility. Preserving fertility is important because these cancers are more common in younger women.

Women with stage II squamous cell cancers who cannot have radiation therapy—perhaps because they had radiation therapy in the past for another cancer—may also have surgery.
The extent of surgery depends on the cancer's stage and size. Types of surgery include
- Laser surgery. This involves using a narrow beam of light to kill cancer. It's often used to treat Stage 0 cancers.
- Loop electroexcision. This involves using low-voltage, high-frequency radio waves in a thin loop of wire to cut away superficial (Stage 0) cancers.
- Radical vaginectomy. Removes the vagina and adjacent tissues.
- Vaginectomy combined with radical hysterectomy. Removes the vagina, uterus, and adjacent tissues.
- Lymphadenectomy. Removes the lymph nodes in the groin or inside the pelvis.
- Pelvic exenteration. This includes radical hysterectomy, vaginectomy, and removal of the bladder, rectum, and part of the colon.
If all or part of the vagina must be removed, it can be reconstructed with tissue from another part of the body.
When To Call a Professional
Contact your doctor if you develop any symptoms of vaginal cancer. Keep in mind that symptoms can be signs of other, less-serious conditions.
You should always call your doctor right away if you have fevers with abdominal or pelvic pain. You might have a serious infection that needs treatment right away.
Because vaginal cancer is relatively rare, seek the opinion of a specialist in gynecological oncology.
Prognosis
The outlook depends on the size and stage of the cancer when it is diagnosed. Early detection and treatment improves the prognosis.
Cervical Cancer
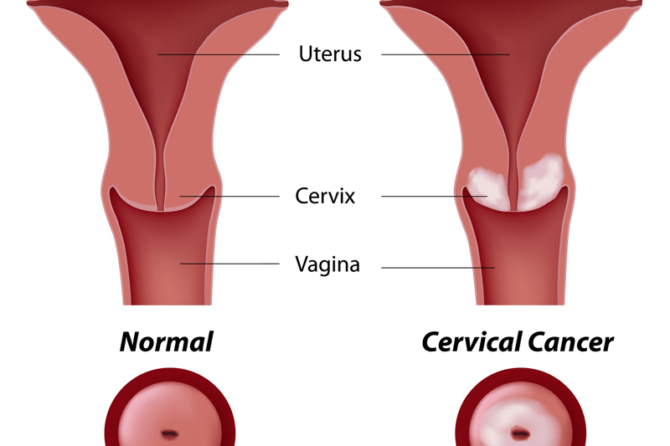
is a type of cancer that occurs in the cells of the cervix — the lower part of the uterus that connects to the vagina.
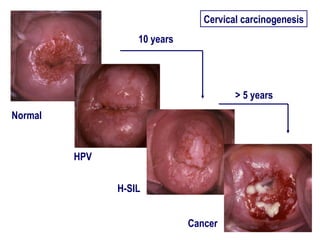
Various strains of the human papillomavirus (HPV), a sexually transmitted infection, play a role in causing most cervical cancer.
When exposed to HPV, the body's immune system typically prevents the virus from doing harm. In a small percentage of people, however, the virus survives for years, contributing to the process that causes some cervical cells to become cancer cells.
You can reduce your risk of developing cervical cancer by having screening tests and receiving a vaccine that protects against HPV infection.
Symptoms
Early-stage cervical cancer generally produces no signs or symptoms.
Signs and symptoms of more-advanced cervical cancer include:
- Vaginal bleeding after intercourse, between periods or after menopause
- Watery, bloody vaginal discharge that may be heavy and have a foul odor
- Pelvic pain or pain during intercourse
When to see a doctor
Make an appointment with your doctor if you have any signs or symptoms that concern you.
Additional Information
National Cancer Institute (NCI)
U.S. National Institutes of Health
Public Inquiries Office
Building 31, Room 10A03
31 Center Drive, MSC 8322
Bethesda, MD 20892-2580
Phone: 301-435-3848
Toll-Free: 1-800-422-6237
TTY: 1-800-332-8615
http://www.nci.nih.gov/
American Cancer Society (ACS)
1599 Clifton Road, NE
Atlanta, GA 30329-4251
Toll-Free: 1-800-227-2345
http://www.cancer.org/